Barriers to Family Planning Use in Rural Uttar Pradesh
In an attempt to understand the reasons for high unmet need in the state, low use of family planning methods and help gain evidence for revising the existing population policy of Uttar Pradesh, SIFPSA carried out a research study in the year 2014-15 to examine the barriers faced in adoption of family planning services, particularly sterilization and IUCD, in rural Uttar Pradesh.
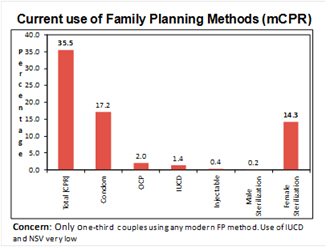
 Uttar Pradesh is the most populous state in the country, and with a TFR of 3.1, the state continues to be on a very high fertility trajectory. Despite all efforts made by the state, only 37 percent of 3.39 crore married eligible couples use any modern family planning method in the state. There are nearly 80 lac eligible couples in UP having unmet need for family planning of which 38 lac (48%) have desired to adopt sterilization to limit their family size and rest have unmet need for spacing. An estimated 252 maternal deaths occur per one lakh live births in Uttar Pradesh due to complications related to pregnancy and childbirth, of which, lack of access to quality family planning services is a major contributing factor. Increasing access to family planning information, services and supplies has dramatic health benefits for women and children. Access to contraceptive choices and ability to act upon those choices are also seen as two most important aspects of a larger 'reproductive rights' framework. Therefore, ensuring access to appropriate, safe and quality family planning choices to all its citizen is one of the most important responsibilities of the state. Uttar Pradesh needs to contribute at least 12.6 million new users to achieve the FP2020 goals set for the state.
Uttar Pradesh is the most populous state in the country, and with a TFR of 3.1, the state continues to be on a very high fertility trajectory. Despite all efforts made by the state, only 37 percent of 3.39 crore married eligible couples use any modern family planning method in the state. There are nearly 80 lac eligible couples in UP having unmet need for family planning of which 38 lac (48%) have desired to adopt sterilization to limit their family size and rest have unmet need for spacing. An estimated 252 maternal deaths occur per one lakh live births in Uttar Pradesh due to complications related to pregnancy and childbirth, of which, lack of access to quality family planning services is a major contributing factor. Increasing access to family planning information, services and supplies has dramatic health benefits for women and children. Access to contraceptive choices and ability to act upon those choices are also seen as two most important aspects of a larger 'reproductive rights' framework. Therefore, ensuring access to appropriate, safe and quality family planning choices to all its citizen is one of the most important responsibilities of the state. Uttar Pradesh needs to contribute at least 12.6 million new users to achieve the FP2020 goals set for the state.
 In such a scenario, there seemed a need to review and revise the existing population Policy. In an attempt to understand the reasons for such high unmet need and low use of family planning methods and help gain evidence for revising the population policy, SIFPSA carried out a research study for examining the barriers faced in adoption of family planning services, particularly sterilization and IUCD, in rural Uttar Pradesh. The study also aimed at understanding the health system's perspective of these barriers and opportunities to overcome them by interacting with frontline health workers, program managers, and policy makers in the state.
In such a scenario, there seemed a need to review and revise the existing population Policy. In an attempt to understand the reasons for such high unmet need and low use of family planning methods and help gain evidence for revising the population policy, SIFPSA carried out a research study for examining the barriers faced in adoption of family planning services, particularly sterilization and IUCD, in rural Uttar Pradesh. The study also aimed at understanding the health system's perspective of these barriers and opportunities to overcome them by interacting with frontline health workers, program managers, and policy makers in the state.
The study drew a large sample size of 2400 eligible women and 600 mothers-in-law from 10 districts namely Rampur, Bahraich, Gonda, Etah, Mainpuri, Pilibhit, Fatehpur, Bareilly, Kanpur Nagar and Mau, randomly selected from a set of 35 districts with low family planning performance, making the findings fairly representative. 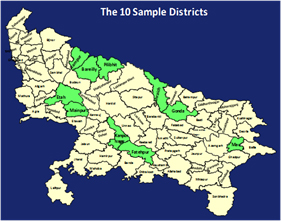 The study also included qualitative discussions with 20 MOICs of Block PHCs and in-depth interviews with 100 ANMs and 113 ASHAs. Discussions were also held with selected state level senior government officials who played a key role in influencing and framing policies in health and family welfare to understand their perspective on family planning, possible barriers in its uptake and solutions for improving family planning usage in the state.
The study also included qualitative discussions with 20 MOICs of Block PHCs and in-depth interviews with 100 ANMs and 113 ASHAs. Discussions were also held with selected state level senior government officials who played a key role in influencing and framing policies in health and family welfare to understand their perspective on family planning, possible barriers in its uptake and solutions for improving family planning usage in the state.
The study revealed several important areas requiring focus, including addressing the prevailing myths and misconceptions amongst the potential clients on adoption of higher order family planning methods.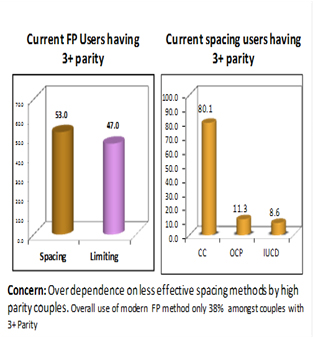 Major reasons for discontinuation by current non-users of any family planning method were quoted as: inconvenient to use, led to illness/weakness, method failure, difficult to obtain, desire for more children etc. Moreover, despite achieving the ideal family size, nearly 31 percent couples had not thought of adopting permanent method, prime reasons being fear of sterilization, loss of stamina after sterilization, opposition from husband/family members, illness/weakness and in some cases it was thought to be against religion
Major reasons for discontinuation by current non-users of any family planning method were quoted as: inconvenient to use, led to illness/weakness, method failure, difficult to obtain, desire for more children etc. Moreover, despite achieving the ideal family size, nearly 31 percent couples had not thought of adopting permanent method, prime reasons being fear of sterilization, loss of stamina after sterilization, opposition from husband/family members, illness/weakness and in some cases it was thought to be against religion
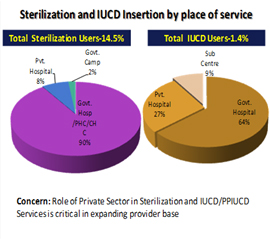
The community level estimates showed that while knowledge of female sterilization was nearly universal, only 68 percent eligible couple had heard of male sterilization. Out of 14.5 percent sterilization users, only 0.2 percent had adopted male sterilization. While almost all ASHAs regularly motivated clients for various spacing methods and female sterilization, only 61 percent reported motivating clients for NSV. Out of 38 percent ASHAs who reported referring a client for male sterilization, 26 percent reported referring them to the district hospital, 12 percent to the block CHC/PHC and none to any private health facility. Major barriers sited for low acceptance of male sterilization clearly hinge on the prevailing myths and misconceptions like- unfit to work after sterilization, opposition by wife, fear of operation, lack of knowledge and reduction in pleasure after sterilization, opposition from family, difficulty in accessing the service etc. This is further corroborated by the fact that only 17 percent PHCs and CHCs had doctors trained in providing NSV services, whereas 91 percent facilities offered regular female sterilization services at the site.
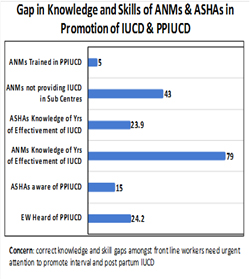 There were many strategic leads that the study had to offer. To state a few, the study clearly indicated the need for a focused inter-personal and intensive communication program to address the prevailing myths, misconceptions, fears and concerns of families and couples towards acceptance of higher order family planning methods like long acting reversible and permanent methods. ASHAs and other frontline health workers need to be adequately trained to provide counselling on elements of continuum of care beginning with ANC and followed through intra and post partum periods. They should also be oriented on behaviour change communication (BCC) skills for dealing with the prevailing myths and misconceptions, particularly concerning long acting reversible and permanent methods of family planning.
There were many strategic leads that the study had to offer. To state a few, the study clearly indicated the need for a focused inter-personal and intensive communication program to address the prevailing myths, misconceptions, fears and concerns of families and couples towards acceptance of higher order family planning methods like long acting reversible and permanent methods. ASHAs and other frontline health workers need to be adequately trained to provide counselling on elements of continuum of care beginning with ANC and followed through intra and post partum periods. They should also be oriented on behaviour change communication (BCC) skills for dealing with the prevailing myths and misconceptions, particularly concerning long acting reversible and permanent methods of family planning.
Mothers-in-law as decision makers in the family continue to be seen influencing the couple's ability in taking decisions for family planning adoption.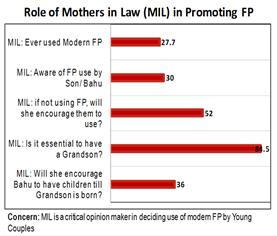 The study suggested a customized communication plan focusing on such influences to be put in place to convert them as family planning champions in the community.
The study suggested a customized communication plan focusing on such influences to be put in place to convert them as family planning champions in the community.
With ever-increasing institutional deliveries, there is a need to focus on post partum family planning for which adequate provision should be made for counselling of women/couples during their hospital stay, motivating them to adopt PPIUCD and post partum sterilization.
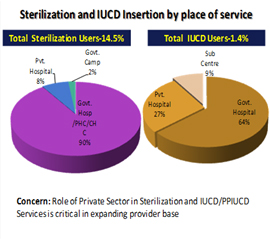 The study also indicated the need to engage private sector health care facilities through accreditation and extending the government scheme for increasing the choice of facilities for the clients to go for higher order family planning services like IUCD and sterilization, with adequate quality of care. The study also suggested that contraceptive technology update program should be made mandatory for program managers, surgeons and field forces to undergo periodically, updating their understanding on various methods.
The study also indicated the need to engage private sector health care facilities through accreditation and extending the government scheme for increasing the choice of facilities for the clients to go for higher order family planning services like IUCD and sterilization, with adequate quality of care. The study also suggested that contraceptive technology update program should be made mandatory for program managers, surgeons and field forces to undergo periodically, updating their understanding on various methods.
 Misconceptions and fears related to family planning methods still persist, limiting the widespread use of modern FP methods. Health providers must also be adequately trained to provide information related to associated side effects of FP methods, enabling them to counsel clients who may experience them. Timely follow up of family planning clients, as per the set protocol of Government of India, must also be ensured. Not providing post service follow up and not attending to any perceived complications may also result in demotivating other potential clients in the vicinity. Hence, post service follow up remains a critical aspect of service standards, needing close monitoring.
Misconceptions and fears related to family planning methods still persist, limiting the widespread use of modern FP methods. Health providers must also be adequately trained to provide information related to associated side effects of FP methods, enabling them to counsel clients who may experience them. Timely follow up of family planning clients, as per the set protocol of Government of India, must also be ensured. Not providing post service follow up and not attending to any perceived complications may also result in demotivating other potential clients in the vicinity. Hence, post service follow up remains a critical aspect of service standards, needing close monitoring.
Strategic behaviour change communication interventions should include targeted campaigns, activities, and accurate messages to correct myths, misconceptions and fears around FP use. The study also highlighted the potential for creating more interactive forums to encourage dialogue and communication around the benefits of family planning and address the socio-cultural barriers to FP use, including strategic engagements with various religious and cultural organizations to include family planning discussions in their activities and forums.
The detailed study report is available at www.sifpsa.org
Best Practices / Ongoing Activities
- Health Partners' Forum - Fostering convergence, maximizing synergies
- Strengthening Implementation of RMNCH+A Health Strategies in UP
- Forging Partnerships for Augmenting Family Planning Performance in UP
- Garnering Support-Reinforcing Commitments: Working with the Village Health Sanitation and Nutrition Committee
- Moving towards excellence: Capacitating ASHA Sanginis for supportive supervision and performance improvement
- Folk Media - Health Messages through Edutainment"Chalo Gaon Ki Oar"
- Newsletter ASHAYEIN
- Lok Geeton Mei Beti English Hindi
- Chalo Gaon Ki Oar English Hindi
- HMIS & MCTS Training cum Review English Hindi
- Clinical Family Planning activities
- Hausala Sajheedari English Hindi
- mSehat English Hindi
- Sampoorna English Hindi
- Sehat Sandeshwahini English Hindi
- Sarthi Sandeshwahini English
- Sunehere Sapne Sanwarti Rahein
- Hausala Training Centres
- World Population Day English Hindi
- Barriers to Family Planning Use in Rural Uttar Pradesh English Hindi
- Out of Pocket Expenditure and Health Seeking Behaviour in Uttar Pradesh English Hindi
- Meri Sehat Mera Nirnay
Get in Touch with us
(Uttar Pradesh), INDIA
E-Mail : info@sifpsa.org
Phone :(91 - 0522) 2630902,997,741,896,899,894
Fax :
Site Manage by : MARG Software Solutions
2016 © SIFPSA All Rights Reserved
Number of Visitors

